Recent improvements in national kidney transplant policy have evened the rates at which African-American, Hispanic and Caucasian transplant candidates receive kidneys from deceased donors, according to data from United Network for Organ Sharing (UNOS). UNOS serves as the national Organ Procurement and Transplantation Network (OPTN) under federal contract.
“This marks a major milestone in transplantation in the United States,” said Mark Aeder, M.D., immediate past chair of the OPTN/UNOS Kidney Transplantation Committee. “For many years African-American and Hispanic candidates weren’t being transplanted at the same rate they represented among patients on the national waiting list. That imbalance has now disappeared.”
The findings stem from a recent analysis of effects of a kidney allocation system (KAS) implemented in December 2014. The new policy was intended to increase equity in access to kidney transplants and promote more effective utilization of available organs. The analysis shows progress on many key goals in the first two years of the new system.
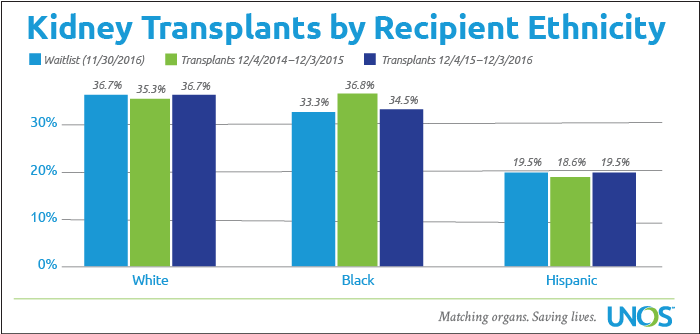
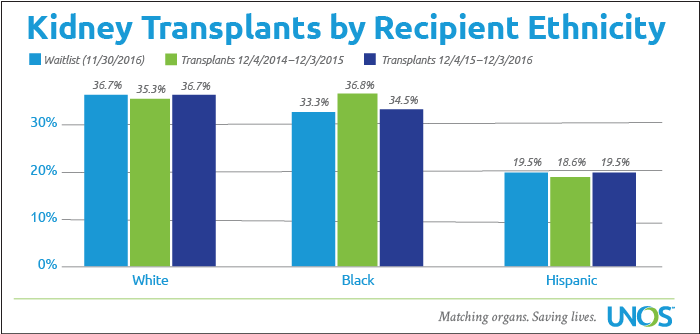
As of November 30, 2016, 36.7 percent of candidates awaiting a kidney transplant were Caucasian, while 36.7 percent of deceased donor kidney recipients from December 2015 through November 2016 were Caucasian. For the same time frames, African-Americans represented 33.3 percent of waitlisted candidates and 34.5 percent of deceased donor kidney recipients; also 19.5 percent of waitlisted kidney candidates were Hispanic, while 19.5 percent of kidney recipients were Hispanic.
“The transplant community has striven for many years to close ethnic gaps between people who are listed for a kidney and those receiving them,” said Jerry McCauley, M.D., M.P.H., FACP, immediate past chair of the OPTN/UNOS Minority Affairs Committee. “African-Americans and Hispanics are at higher risk for developing end-stage kidney disease than other ethnicities, and thus they’re listed for kidney transplantation at a rate higher than they represent in the U.S. population. KAS appears to have closed the final policy gap. Minority candidates still face challenges, as they often are not referred for transplant as quickly as others and can take longer to complete their evaluations. Once they are listed, the new allocation system provides equal access to transplantation.”
“This is an important achievement not only for minority candidates, but for trust in the national transplant system,” said Sylvia Rosas, M.D., MSCE, chair of the OPTN/UNOS Minority Affairs Committee. “Everyone needing a transplant depends on someone else’s personal decision to become an organ donor. It helps in donor education and outreach to know that our diverse communities have a fair chance to benefit from a transplant.”
One factor accounting for part of the change is a rising trend of deceased donation among African-Americans and Hispanics, which provides more transplant opportunities for minority candidates. “It’s not essential to match the ethnicity of donors and recipients,” said Dr. McCauley, “but people who share a similar heritage sometimes are more immunologically compatible.
“About 20 years ago,” Dr. McCauley continued, “African-Americans and Hispanics donated organs at a rate somewhat lower than they represented in the U.S. population. Today the ethnic makeup of donors is essentially the same as the population. This reflects the success of outreach by many organizations and donation advocates to engage minority communities and address their specific questions and concerns about the donation process. The OPTN/UNOS Minority Affairs Committee has also worked for many years to ensure the unique needs and perspectives of minority populations are fully considered by the transplant community.”
UNOS, in its role as the OPTN, has continued over time to refine kidney allocation policy to improve equitable access to transplantation. Prior to KAS implementation, several changes to kidney allocation policy have reflected emerging science in histocompatibility and immunology – the matching of immune system compatibility between organ donors and recipients.
“Our immune system represents one of the most complex biological processes known to man,” said Robert Bray, Ph.D., chair of the OPTN/UNOS Histocompatibility Committee. “Immune system compatibility between a donor and recipient is important in all of transplantation, but it’s most critical for the success of kidney and pancreas transplantation. Over the past 25 years, we have made great strides in our understanding of the specific aspects of immune system compatibility that have greatest impact on transplant success, as well as major advances in immune-suppressing medications to combat rejection once transplanted.
“When the national transplant network began in the late 1980s, complete immunologic matching was believed to be required,” said Dr. Bray. “Over the years, our research has shown us two important things. First, selected aspects of immune compatibility seem to be most important. Second, requiring complete compatibility matching could disadvantage minority candidates as ethnic heritage can influence what antigens – immune system markers – we each have. Since the great majority of deceased donors were Caucasian, it was likely that they would not match as closely with candidates of other ethnic groups.
“Several times over the last two decades, we’ve refined kidney policy to give allocation priority to those immunological combinations that are most likely to result in a long-term successful transplant,” Dr. Bray added. “These changes, combined with policy changes related to how we assess waiting time and how we prioritize access for the highly sensitized candidate, have all broadened the opportunity for minority patients to be considered for the available kidneys.”
While the current data are encouraging, “Much more work needs to be done,” noted Dr. Aeder. “We’ve improved transplant access for the ethnic groups that make up the great majority of the waiting list. But there is still a noticeable gap between listing and transplant rates for people of Asian heritage. We will continue to study how to improve access for everyone, regardless of ethnicity, age or other factors.
“And our greatest challenge – ensuring everyone who needs a transplant can receive one – is still uppermost for us,” added Dr. Aeder. “The good news is that through increases in the selfless gift of organ donation, we are transplanting more people each year. In fact, in the two years since KAS was implemented, kidney transplantation has increased more than nine percent nationwide. But tens of thousands of people remain in need today. We rely on the public’s commitment to help them through organ donation.”