Living with devices
Heart devices
Today, there are treatments for some types of end-stage organ disease that replace the functions of the failing organ(s). By learning about your choices, you can work with your doctor to determine the most appropriate course of treatment.
Artificial hearts

Sometimes referred to as a “bridge-to-transplant,” artificial hearts are composed of plastic, aluminum and polyester, and perform an action similar to the natural heart.An external power system energizes and regulates the artificial pump through a system of compressed air hoses that enter the heart through the chest.
LVADs
![By National Heart Lung and Blood Institute (NIH) (National Heart Lung and Blood Institute (NIH)) [Public domain], via Wikimedia Commons Left ventricular device. Source: Public domain - NIH](https://transplantliving.org/wp-content/uploads/sites/2/lvad.png)
Sometimes used as a “bridge-to-transplant” or as a permanent therapy alternative called “destination therapy,” the LVAD is a mechanical pump-type device that is surgically implanted to help maintain the pumping ability of a heart that is unable to effectively function on its own. These mechanical heart pumps can significantly improve a patient’s health and survival rate.
One typical type of LVAD involves a tube connected to the left ventricle that directs blood from the ventricle into a pump. The pump then sends blood into the aorta (the large blood vessel leaving the left ventricle), which effectively bypasses the weakened ventricle.
ICDs
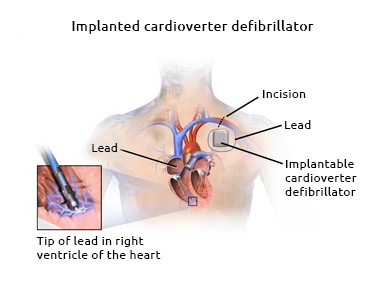
ICDs are pacemaker-like devices that continuously monitor the heart’s rhythm, and deliver life-saving shocks if a dangerous heart rhythm is detected. ICDs are placed in the hearts of people who have had certain abnormal heart rhythms (arrhythmias). The first full human implantation of an ICD occurred in February 1980. The device has been improved since then to identify arrhythmias and provide electrical shocks to restore normal rhythm.
An ICD is connected to leads positioned inside the heart or on its surface. These leads are tunneled to a pulse generator, which is implanted in a pouch beneath the skin of the chest of abdomen. Newer devices are smaller and have simpler lead systems, which can be installed through blood vessels, therefore eliminating the need for open-chest surgery.
Pacemakers
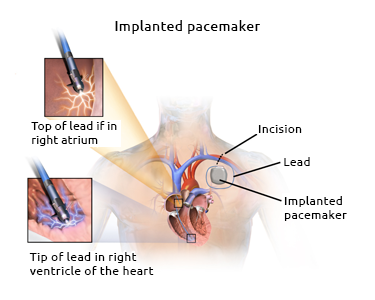
An artificial pacemaker is a small battery-operated device that helps the heart beat at a regular rhythm. Some are internal and permanent, while others can be temporary and external. Both use batteries to send small electrical impulses from an electrode placed next to the heart wall to help it pump properly.
Kidney devices
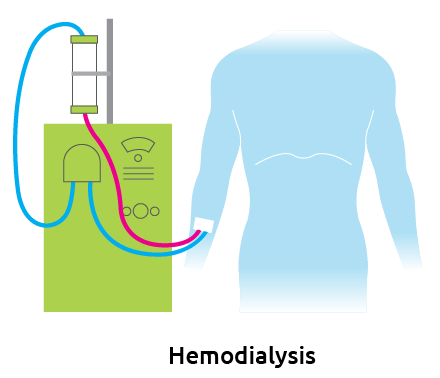
Hemodialysis
Hemodialysis is the most common method used to treat advanced and permanent kidney failure. It involves a coordinated effort from you, your family and your entire health care team, including your nephrologist, dialysis nurse, dialysis technician, dietician and social worker. In hemodialysis, your blood passes through a machine with a special filter, a few ounces at a time, to remove excess fluid and wastes.
The procedure, done at home or at a dialysis center, usually takes about three or four hours per session and typically occurs three times per week. For hemodialysis to occur, a special site, called an access, must be surgically created in the arm, leg or near the collarbone. These access sites are used to remove blood from the body and return it after the filtration process has been completed.
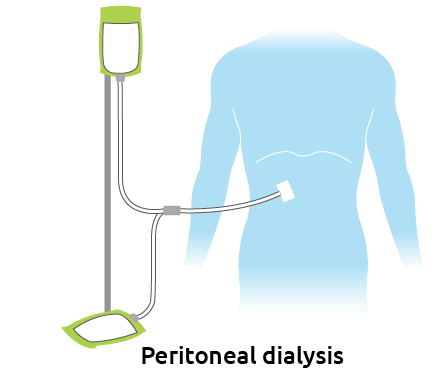
Peritoneal dialysis
Another way to remove wastes from the blood is a process called peritoneal dialysis (PD). The walls of the abdominal cavity are lined with a membrane called the peritoneum. During PD, a mixture of sugar, salt and other minerals dissolved in water, called dialysis solution, is placed in a person’s abdominal cavity through a catheter. The body’s peritoneal membrane enclosing the digestive organs allows waste products and extra body fluid to pass from the blood into the dialysis solution.
These wastes then leave the body when the used solution is drained from the abdomen. Each cycle of filling and draining is called an exchange. There are three types of peritoneal dialysis, which differ mainly in the schedule of exchanges. Talk with your doctor about which type best suits your lifestyle.
